Awakenings True Story—what really happened
“Awakenings True Story” refers to the extraordinary real-life events behind the 1990 film Awakenings, which dramatized a chapter of modern neurology that seemed almost miraculous: patients who had been frozen for decades by a mysterious post-encephalitic condition suddenly “woke up” after receiving a Parkinson’s drug, L-DOPA. For a brief window, they ate, danced, joked, remembered, and rejoined life—only to face complications that were as sobering as the initial results were dazzling.
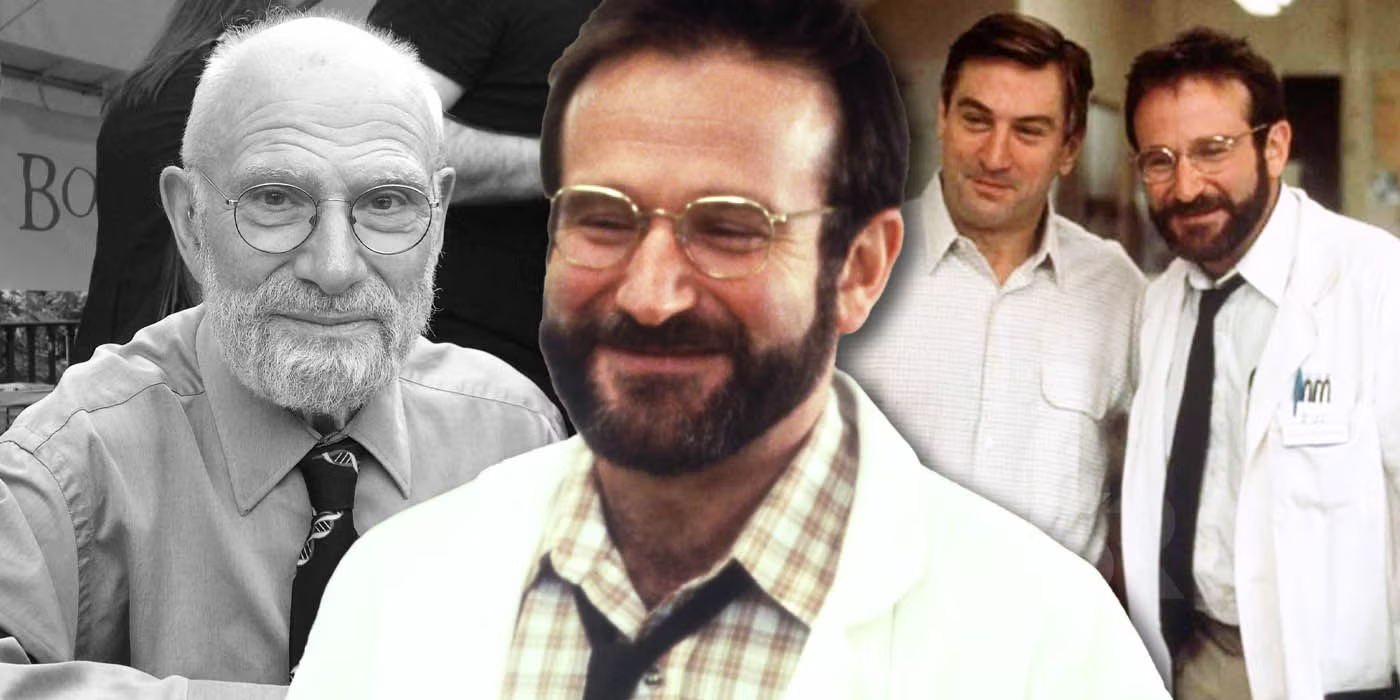
At the heart of the Awakenings True Story is a physician and writer, modeled in the movie as Dr. Malcolm Sayer but based on the real neurologist Dr. Oliver Sacks. In the late 1960s, he began treating a cohort of long-term patients who had survived the 1917–1928 encephalitis lethargica pandemic. They were alive, but almost entirely motionless—sometimes able to track with their eyes or respond in minimal ways, yet fundamentally cut off from the fluent movements, speech, and spontaneity most of us take for granted.
When L-DOPA became available as a therapy for Parkinson’s disease, Sacks saw a daring possibility. If the patients’ problem involved dopamine-starved motor circuits—rigid, masked, untalking—then L-DOPA might rekindle movement. He carefully introduced the drug at low doses and watched, sometimes in awe, as those who had been still for decades began to stir. The Awakenings True Story is thus not only a medical tale but a human one, full of the shock of rediscovery: a delayed adolescence, a sudden middle age snatched from time’s deep freeze, a reckoning with lost years, families, and identities.
Yet the same story refuses easy triumph. The awakenings were often partial and transient. As doses rose, so did complications: tics, dyskinesias (uncontrollable movements), mood swings, compulsions, and paradoxically, the return of rigidity once tolerance set in. The Awakenings True Story lands us in medicine’s most difficult terrain: how to weigh a brilliant but unstable benefit against burdensome side effects—especially for people who had waited half a lifetime for motion and meaning.
The medical backstory behind Awakenings True Story
To understand the Awakenings True Story, it helps to revisit the earlier medical mystery: encephalitis lethargica, sometimes called “sleepy sickness.” During and after World War I, clinicians worldwide documented a wave of encephalitis with protean symptoms—profound sleepiness, movement disorders, psychiatric changes, and, in some survivors, a chronic post-encephalitic parkinsonism. Many patients eventually stabilized into states of extreme motor poverty: masked faces, barely audible voices, catatonia-like stillness, waxy flexibility, and “statue” poses they could not escape.
Over the decades, caregivers created lives of ritual, habit, and modest stimulation for these patients in chronic hospitals. They were not absent; they lived within—patients sometimes knew exactly what was happening but could not translate intent into action. Nurses learned to read tiny signals: a blink for yes, a sidelong glance for discomfort, a subtle shift of the eyes that meant “stay,” “sit,” “thank you.” The Awakenings True Story is therefore also a story of invisible expertise: the compassion and pattern-recognition of people who never appeared on movie posters but sustained human dignity through drudgery and love.
Then came dopamine. Mid-20th-century neuroscience began to map neurotransmitters; dopamine emerged as a key regulator of the basal ganglia, the brain’s movement circuits. Parkinson’s disease was associated with dopamine deficiency in the substantia nigra. L-DOPA, a dopamine precursor, could cross the blood–brain barrier and replenish dopamine in those circuits. Clinicians watched tremors quiet, gait improve, faces animate. That success emboldened Sacks and others to try L-DOPA on post-encephalitic patients whose states resembled a supercharged parkinsonism.
The Awakenings True Story unfolded as a sequence of cautious experiments. Each patient had a unique neurological geography—no two brains, no two decades of stillness, were alike. Some needed small doses to spark; others required slow, persistent titration. For a stunning interval, ward rooms became ballrooms. People who had not stood up in years walked. They asked for radios, newspapers, and mirrors. They held hands with visitors who had grown grey while they remained statues. The joy was real, and so were the tears that followed when instability intruded: dyskinesias that flung arms like whips, floods of speech that made sleep impossible, and psychological upheavals as patients confronted the sudden return of agency.
From memoir to movie—what the film changed
The film Awakenings, with Robin Williams as the Sacks-inspired doctor and Robert De Niro as the patient Leonard Lowe (based on “Leonard L.”), introduced the Awakenings True Story to a global audience. It captured the wonder of first movement—the halting smile, the daring step—and the ethical difficulty of giving and then partly taking away a world. But like all adaptations, it shaped reality for narrative clarity.
First, the timeline compresses. In real life, awakenings unfolded over weeks and months, with doses adjusted, side effects tracked, and lives reorganized around the new volatility. The film must condense arcs so that a viewer can watch hope ignite and falter within two hours. That compression amplifies the emotional whiplash and makes the reversal feel more sudden than many clinical courses actually were.
Second, individual stories are merged. The film’s Leonard Lowe is a composite, carrying experiences drawn from multiple patients. That does not falsify the Awakenings True Story, but it focuses attention on one relationship to illuminate broader truths. It also means that some extraordinary but idiosyncratic details—patients who wrote poems, developed new tics, fell in love with jukebox songs—are redistributed or omitted.
Third, medical nuance is simplified. The film rightly shows that L-DOPA is not a magic bullet; still, some complexities—like dose-response hysteresis, diurnal fluctuations, paradoxical kinesia (brief bursts of normal movement), and the delicate dance of adding adjunct medications—would bewilder a general audience. For clarity, the movie leans on visible cues: a hand that stops shaking, a smile that breaks across a once-masked face, a dyskinetic wave that signals trouble returning.
Finally, the movie centers the doctor-patient dyad in a way that eclipses the ecosystem. In the Awakenings True Story, nurses were indispensable, family members were protagonists, and administrators, pharmacists, and therapists all shaped outcomes. Cinema demands focus; reality required a village.
These divergences don’t diminish the Awakenings True Story. If anything, they underscore its richness: the film offers a doorway, and the deeper medical literature—and Sacks’s own pages—offer rooms beyond.
The science and ethics inside Awakenings True Story
The Awakenings True Story is a case study in how neurochemistry meets lived experience. On the scientific side, L-DOPA demonstrates that restoring a missing neurotransmitter can reboot circuits, but not always smoothly. Dopamine pathways regulate not only movement but motivation, reward, and impulse control. Too little dopamine, and initiation collapses; too much or too rapidly, and the system oscillates, producing tics, compulsions, insomnia, even psychosis-like symptoms in vulnerable patients. The sweet spot is narrow and moves with time.
Therapeutically, clinicians faced four intertwined challenges:
- Titration and tolerance. Patients might respond at one dose and then require more, entering a cycle where benefit and side effects chase each other. Over months, some experienced diminishing returns; others could be “re-awakened” with modifications.
- Individual variability. The “same” syndrome in two patients could respond very differently. Patterns of brain injury from encephalitis, differences in metabolism, and coexisting conditions created unique response curves.
- Behavioral and psychological adaptation. Imagine being locked in your body for decades and then suddenly set into motion. Desire, grief, anger, romance, creativity, and fear all rush back. Some patients embraced the storm; others were overwhelmed, especially when oscillations made the self feel unreliable.
- Systems of care. The best outcomes demanded interdisciplinary teams. Physical therapists retrained muscles, speech therapists coaxed voices, occupational therapists rebuilt daily routines, and nurses spotted early signs of brewing dyskinesias or emotional crashes.
Ethically, the Awakenings True Story sharpened enduring questions. Is a brilliant but brief awakening worth the turbulence that may follow? Who decides—the patient, the family, the physician—and how do they decide for people whose capacity fluctuates day to day? What constitutes “success”: a few months of full presence, or a sustainable modest improvement? Should clinicians accept a controlled degree of side effects to preserve a patient’s preferred balance of freedom and fatigue?
In practice, consent was an ongoing conversation. Some patients chose to continue, accepting risk for the sake of autonomy and joy. Others preferred stability over extremes. The ethical gold standard was—and remains—attention to the person’s values, revisited as conditions evolve.
Why Awakenings True Story still matters
Decades later, the Awakenings True Story continues to ripple through medicine and culture. Clinically, it prompted deeper inquiry into post-encephalitic states, catatonia, Parkinsonism, and the nuanced roles of dopamine. It also reshaped how chronic-care institutions think about stimulation, agency, and the presumption of inner life. Even when bodies barely move, minds may be present; care plans should be structured to assume personhood, not its absence.
Scientifically, the saga helped broaden interest in neuromodulation—how to nudge brain circuits with pharmaceuticals, stimulation, or behavioral cues to recover lost function. While encephalitis lethargica itself is exceedingly rare today, analogous problems persist: severe Parkinson’s disease with freezing of gait, prolonged hypoactive states after brain injury, or catatonia linked to psychiatric or medical causes. The Awakenings True Story taught clinicians to look for “movement within stillness,” to test small doses, and to scaffold any pharmacologic boost with rehabilitation that consolidates gains.
Culturally, the story stands as a parable of humility. Medicine can deliver marvels—and limits. The world greeted the initial awakenings with headlines that promised new beginnings; then it largely looked away when the long work of management began. The fuller telling resists both hype and cynicism. The awakenings were real. So were the relapses, accommodations, half-victories, and stubborn joys that followed.
On a human level, the Awakenings True Story asks each of us to rethink what counts as a life worth living. For some patients, even a partial return to conversation—to say “good morning,” to choose music, to ask for a favorite food—was a triumph. For others, the roller coaster was too much. Recognizing that diversity of good outcomes is part of honoring personhood.
Finally, the story endures because it models a way of seeing. The doctor in Awakenings is curious, patient, and emotionally available; he observes small things and tries modest changes before grand ones. That posture—attentive, experimental, collaborative—is medicine at its best. The Awakenings True Story invites caregivers, families, and communities to keep that posture even when cameras turn away.
Lessons for today from Awakenings True Story
The Awakenings True Story offers a toolkit we can still use:
Look for reversibility. Even in long-standing conditions, there may be reversible components—neurochemical bottlenecks, under-stimulated circuits, environmental barriers. Gentle trials with clear stop rules can reveal hidden capacity.
Favor interdisciplinary care. A medication can open a door; therapy helps a person walk through it and stay inside the room. Pair pharmacology with physical, speech, and occupational plans from the outset.
Co-create definitions of success. Outcomes should be measurable but personal: a daily walk to the garden, a conversation at dinner, a favorite hobby reclaimed. In the Awakenings True Story, goals that mattered to patients were often modest and luminous.
Expect adaptation. Brains and drugs dance. Doses that work now may not work next month. Build flexible regimens, frequent check-ins, and shared decision-making into the plan.
Honor the quiet work. Celebrate nurses, aides, and families who notice the five-second window when a cue can become a step. The Awakenings True Story is made of such noticing.
These principles extend beyond neurology, into rehab after strokes, post-ICU recovery, and even mental health care where activation and agency can flicker. The enduring gift of the Awakenings True Story is a renewed respect for small experiments and big compassion.
FAQs about Awakenings True Story
1) What does “Awakenings True Story” actually refer to?
It refers to the real clinical episodes behind Awakenings, in which post-encephalitic patients in the late 1960s experienced dramatic, if often temporary, improvements after treatment with L-DOPA.
2) Was there really a doctor like Malcolm Sayer?
Yes. The character is based on neurologist Oliver Sacks, who documented these cases and the complexities that followed the initial successes.
3) Did patients truly “wake up” after decades?
Many did, to varying degrees—speaking, walking, and engaging again—but responses differed widely and often fluctuated over time.
4) How long did the awakenings last?
Durations varied. Some improvements lasted months; others waxed and waned. Side effects and tolerance often limited long-term stability.
5) Why did L-DOPA help?
It replenished dopamine in brain circuits controlling movement, temporarily restoring initiation and fluidity in some patients whose systems were dopamine-starved.
6) Why did problems reappear?
Dopamine pathways are delicate. Over time, tolerance, dyskinesias, mood changes, and sleep disruption could erode the initial gains.
7) Is encephalitis lethargica still around?
The historic pandemic has not recurred at that scale, but sporadic cases and related syndromes exist; however, post-encephalitic parkinsonism like in the story is now rare.
8) Did the film Awakenings change facts?
It compressed timelines, merged patients, and simplified some medical details for narrative clarity, while honoring the core truth of the events.
9) Were the emotional reactions exaggerated for cinema?
The emotions were real, but the pace of change is faster on screen. In life, adaptations unfolded over weeks and months.
10) Could modern medicine handle this better now?
We have more adjuncts, better rehab protocols, and deeper experience with dopaminergic side effects, but the core dilemmas—benefit vs. burden—remain.
11) What role did nurses and therapists play?
A central one. They saw day-to-day patterns, caught early warning signs, and helped translate new movement into meaningful function.
12) Were families prepared for the awakenings?
Often not. Joy mixed with shock, grief for lost decades, and the challenge of re-establishing relationships with someone suddenly in motion again.
13) Did every patient want to continue treatment?
No. Some chose to taper when side effects outweighed benefits; others preferred to keep going despite volatility.
14) Could lower doses have kept benefits longer?
Sometimes smaller, steadier doses helped; in other cases, diminishing returns or side effects still intruded. There was no universal formula.
15) Is L-DOPA the only option for such states?
For post-encephalitic parkinsonism, L-DOPA was the key lever in the Awakenings True Story. Today, clinicians also consider other meds and non-drug therapies case by case.
16) What ethical issues are most prominent?
Informed consent under fluctuating capacity, defining success, managing expectations, and respecting patient preferences amid uncertainty.
17) Did any patients maintain long-term gains?
Some maintained partial improvements with careful management and therapy. Most experienced variability rather than a permanent transformation.
18) How did the Awakenings True Story influence culture?
It broadened public understanding of neurological illness, inspired caregiving empathy, and highlighted the dignity and complexity of people in chronic care.
19) What can caregivers learn from it?
Observe closely, try small, reversible steps, build interdisciplinary support, and co-create goals that reflect the person’s own values.
20) Why does “Awakenings True Story” still resonate?
Because it combines wonder with truth: a glimpse of what medicine can ignite, and a reminder to stand with people when the miracle becomes everyday work.